Fill a Valid Annual Physical Examination Form
The Annual Physical Examination form serves as a crucial tool in facilitating comprehensive health assessments for individuals. Designed to gather essential information prior to a medical appointment, the form requires personal details such as name, date of birth, and address, ensuring that healthcare providers have accurate patient identification. It prompts patients to disclose significant health conditions and a detailed medical history, including current medications and any allergies, which can influence treatment decisions. Additionally, the form includes sections for immunization records and tuberculosis screening, vital for public health and individual safety. A thorough evaluation of various body systems, including cardiovascular and respiratory health, is mandated, allowing for a holistic view of the patient’s well-being. Furthermore, it addresses necessary diagnostic tests, hospitalizations, and surgical procedures, providing a complete medical picture. Recommendations for health maintenance, dietary considerations, and activity restrictions are also integral components, empowering patients to take charge of their health. By completing this form, individuals contribute to a streamlined and effective healthcare experience, minimizing the need for return visits and enhancing overall patient care.
Additional PDF Templates
Acord Binder - The Acord 50 WM is designed for ease of use, providing clear sections and instructions.
When considering the purchase or sale of a mobile home in Ohio, it is vital to utilize the proper documentation to protect both parties involved. The Ohio Mobile Home Bill of Sale form is an essential instrument in this process, ensuring that all relevant details of the transaction are recorded clearly. For further information and access to necessary forms, you can visit All Ohio Forms, which offers a comprehensive range of resources to assist in this important legal matter.
Act of Donation Form Louisiana - The Louisiana act of donation is widely recognized and respected, supporting smooth transactions between parties.
Similar forms
-
Patient Intake Form: Similar to the Annual Physical Examination form, a patient intake form collects essential information about a patient’s medical history, current medications, and allergies. Both documents aim to gather comprehensive data to ensure that healthcare providers have a complete understanding of the patient’s health before any examination or treatment.
-
Consent for Treatment Form: This document is crucial for obtaining a patient’s permission before any medical procedure. Like the Annual Physical Examination form, it ensures that patients are fully informed about their care, which helps in fostering trust and transparency in the healthcare relationship.
- Quitclaim Deed Form: When transferring property ownership, consider utilizing our informative Quitclaim Deed resources to ensure a clear understanding of the process.
-
Immunization Record: An immunization record details a patient’s vaccination history. It parallels the Annual Physical Examination form in that both documents track important health information that can impact a patient’s overall health and readiness for certain medical procedures.
-
Health History Questionnaire: This form gathers information about a patient’s past medical issues and family health history. Similar to the Annual Physical Examination form, it helps healthcare providers assess risk factors and tailor care plans accordingly.
-
Lab Test Requisition Form: This document is used to order specific laboratory tests. Like the Annual Physical Examination form, it includes sections for patient identification and relevant medical history, ensuring that the lab results are interpreted in the context of the patient’s overall health.
Document Example
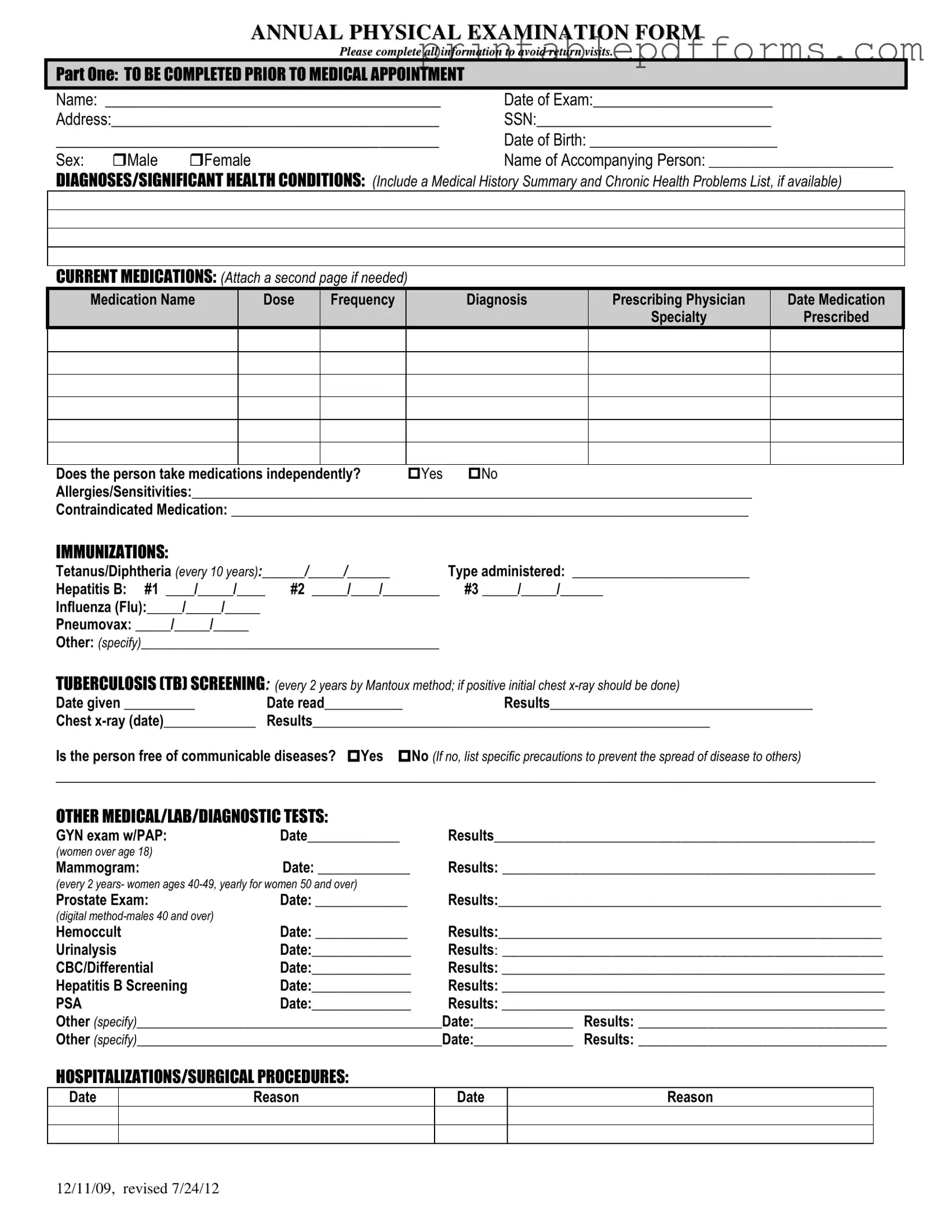
ANNUAL PHYSICAL EXAMINATION FORM
Please complete all information to avoid return visits.
PART ONE: TO BE COMPLETED PRIOR TO MEDICAL APPOINTMENT
Name: ___________________________________________ |
Date of Exam:_______________________ |
Address:__________________________________________ |
SSN:______________________________ |
_____________________________________________ |
Date of Birth: ________________________ |
||
Sex: |
Male |
Female |
Name of Accompanying Person: __________________________ |
DIAGNOSES/SIGNIFICANT HEALTH CONDITIONS: (Include a Medical History Summary and Chronic Health Problems List, if available)
CURRENT MEDICATIONS: (Attach a second page if needed)
Medication Name |
Dose |
Frequency |
Diagnosis |
Prescribing Physician |
Date Medication |
|
|
|
|
Specialty |
Prescribed |
Does the person take medications independently? |
Yes |
No |
Allergies/Sensitivities:_______________________________________________________________________________ |
||
Contraindicated Medication: _________________________________________________________________________
IMMUNIZATIONS:
Tetanus/Diphtheria (every 10 years):______/_____/______ |
Type administered: _________________________ |
|
Hepatitis B: #1 ____/_____/____ |
#2 _____/____/________ |
#3 _____/_____/______ |
Influenza (Flu):_____/_____/_____ |
|
|
Pneumovax: _____/_____/_____ |
|
|
Other: (specify)__________________________________________ |
|
|
TUBERCULOSIS (TB) SCREENING: (every 2 years by Mantoux method; if positive initial chest |
||
Date given __________ |
Date read___________ |
Results_____________________________________ |
Chest |
Results________________________________________________________ |
|
Is the person free of communicable diseases? Yes No (If no, list specific precautions to prevent the spread of disease to others)
_________________________________________________________________________________________________________
OTHER MEDICAL/LAB/DIAGNOSTIC TESTS:
GYN exam w/PAP: |
Date_____________ |
Results_________________________________________________ |
(women over age 18) |
|
|
Mammogram: |
Date: _____________ |
Results: ________________________________________________ |
(every 2 years- women ages
Prostate Exam: |
Date: _____________ |
Results:______________________________________________________ |
|
(digital |
|
|
|
Hemoccult |
Date: _____________ |
Results:______________________________________________________ |
|
Urinalysis |
Date:______________ |
Results: _________________________________________________ |
|
CBC/Differential |
Date:______________ |
Results: ______________________________________________________ |
|
Hepatitis B Screening |
Date:______________ |
Results: ______________________________________________________ |
|
PSA |
Date:______________ |
Results: ______________________________________________________ |
|
Other (specify)___________________________________________Date:______________ |
Results: ________________________________ |
||
Other (specify)___________________________________________Date:______________ |
Results: ________________________________ |
||
HOSPITALIZATIONS/SURGICAL PROCEDURES:
Date
Reason
Date
Reason
12/11/09, revised 7/24/12

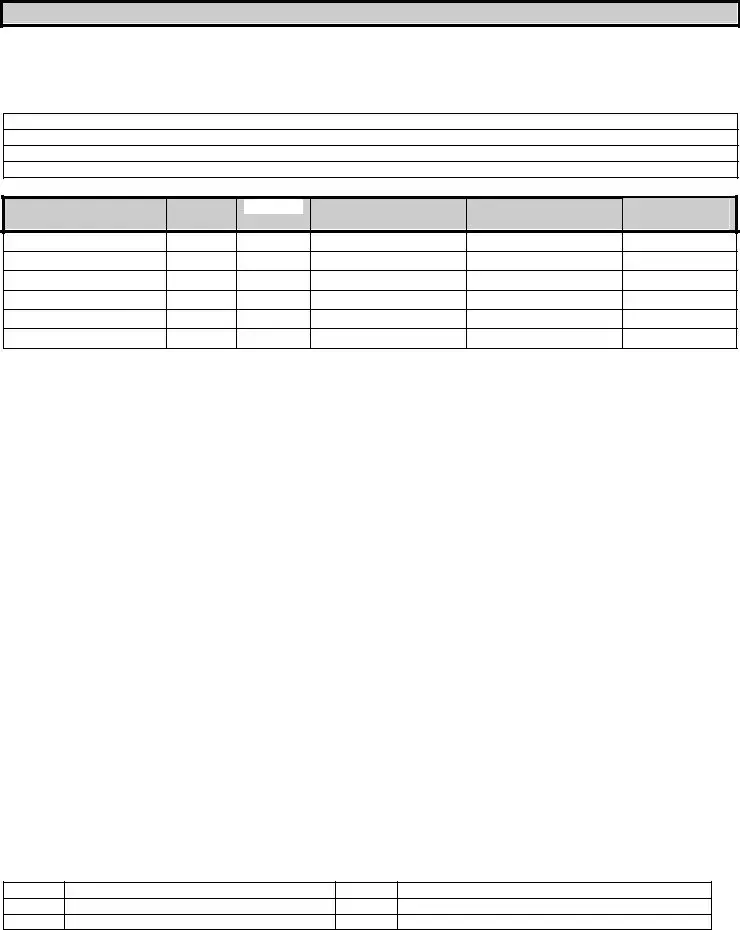
PART TWO: GENERAL PHYSICAL EXAMINATION
|
|
|
|
|
Please complete all information to avoid return visits. |
|
|
|
|
|
Blood Pressure:______ /_______ Pulse:_________ |
Respirations:_________ Temp:_________ Height:_________ |
Weight:_________ |
||||
|
|
EVALUATION OF SYSTEMS |
|
|
|
|
||
|
|
|
|
|
|
|
||
|
|
System Name |
|
Normal Findings? |
Comments/Description |
|
||
|
|
Eyes |
|
Yes |
No |
|
|
|
|
|
Ears |
|
Yes |
No |
|
|
|
|
|
Nose |
|
Yes |
No |
|
|
|
|
|
Mouth/Throat |
|
Yes |
No |
|
|
|
|
|
Head/Face/Neck |
|
Yes |
No |
|
|
|
|
|
Breasts |
|
Yes |
No |
|
|
|
|
|
Lungs |
|
Yes |
No |
|
|
|
|
|
Cardiovascular |
|
Yes |
No |
|
|
|
|
|
Extremities |
|
Yes |
No |
|
|
|
|
|
Abdomen |
|
Yes |
No |
|
|
|
|
|
Gastrointestinal |
|
Yes |
No |
|
|
|
|
|
Musculoskeletal |
|
Yes |
No |
|
|
|
|
|
Integumentary |
|
Yes |
No |
|
|
|
|
|
Renal/Urinary |
|
Yes |
No |
|
|
|
|
|
Reproductive |
|
Yes |
No |
|
|
|
|
|
Lymphatic |
|
Yes |
No |
|
|
|
|
|
Endocrine |
|
Yes |
No |
|
|
|
|
|
Nervous System |
|
Yes |
No |
|
|
|
|
|
VISION SCREENING |
|
Yes |
No |
Is further evaluation recommended by specialist? |
Yes |
No |
|
|
HEARING SCREENING |
|
Yes |
No |
Is further evaluation recommended by specialist? |
Yes |
No |
|
|
ADDITIONAL COMMENTS: |
|
|
|
|
|
|
|
|
|
|
|
|
|
||
|
|
Medical history summary reviewed? |
Yes |
No |
|
|
||
Medication added, changed, or deleted: (from this appointment)__________________________________________________________
Special medication considerations or side effects: ________________________________________________________________
Recommendations for health maintenance: (include need for lab work at regular intervals, treatments, therapies, exercise, hygiene, weight control, etc.)
___________________________________________________________________________________________________________
Recommendations for manual breast exam or manual testicular exam: (include who will perform and frequency)____________________
___________________________________________________________________________________________________________
Recommended diet and special instructions: ____________________________________________________________________
Information pertinent to diagnosis and treatment in case of emergency:
___________________________________________________________________________________________________________
Limitations or restrictions for activities (including work day, lifting, standing, and bending): No Yes (specify)
___________________________________________________________________________________________________________ |
|||
Does this person use adaptive equipment? |
No |
Yes (specify):________________________________________________ |
|
Change in health status from previous year? No |
Yes (specify):_________________________________________________ |
||
This individual is recommended for ICF/ID level of care? (see attached explanation) Yes |
No |
||
Specialty consults recommended? No |
Yes (specify):_________________________________________________________ |
||
Seizure Disorder present? No Yes (specify type):__________________________________ Date of Last Seizure: ______________ |
|||
________________________________ |
_______________________________ |
_________________ |
|
Name of Physician (please print) |
Physician’s Signature |
|
Date |
Physician Address: _____________________________________________ |
Physician Phone Number: ____________________________ |
||
12/11/09, revised 7/24/12
Form Specs
| Fact Name | Description |
|---|---|
| Purpose | The Annual Physical Examination form is used to collect comprehensive health information prior to a medical appointment. |
| Patient Information | Patients must provide personal details such as name, date of birth, and address to ensure accurate medical records. |
| Medication Details | Current medications, including dosages and prescribing physicians, should be listed to inform healthcare providers about the patient's treatment. |
| Immunization Records | Patients must document immunizations, including dates and types, to ensure they are up to date on vaccinations. |
| TB Screening | TB screening is required every two years, with results documented to assess communicable disease risks. |
| GYN and Prostate Exams | Women over 18 should have GYN exams with PAP smears, while men over 40 should have prostate exams, as part of routine health checks. |
| Vital Signs | Blood pressure, pulse, and other vital signs must be recorded to evaluate the patient's overall health status during the exam. |
| Evaluation of Systems | Healthcare providers assess various body systems, noting normal findings or concerns, to provide a thorough health evaluation. |
| Recommendations | The form includes space for recommendations regarding health maintenance, dietary needs, and any necessary follow-up care. |
| State-Specific Laws | Some states may have specific laws governing the use of Annual Physical Examination forms, such as HIPAA compliance and patient privacy regulations. |
Crucial Questions on This Form
What is the purpose of the Annual Physical Examination form?
The Annual Physical Examination form is designed to collect essential health information before a medical appointment. It ensures that your healthcare provider has a comprehensive understanding of your medical history, current medications, allergies, and any significant health conditions. This information helps in providing personalized care and addressing your specific health needs during the examination.
What information do I need to provide in the form?
You will need to fill out various sections of the form, including:
- Your personal details such as name, date of birth, and address.
- A summary of your medical history and any chronic health problems.
- A list of current medications, including dosages and prescribing physicians.
- Details about immunizations and any allergies or sensitivities.
- Results from any recent medical tests or screenings.
Completing all sections thoroughly can help avoid the need for additional visits.
How often should I complete this form?
The Annual Physical Examination form should be completed once a year or whenever you have a significant change in your health status. Regular updates ensure that your healthcare provider has the most current information, which is vital for effective treatment and care.
What should I do if I have questions while filling out the form?
If you have any questions or need assistance while completing the form, do not hesitate to reach out to your healthcare provider's office. They can provide guidance and clarification on any section of the form. It’s important to ensure that all information is accurate and complete to facilitate your medical appointment.
What happens if I do not complete the form?
Failing to complete the Annual Physical Examination form may lead to delays in your appointment. Incomplete forms can result in the need for additional visits to gather necessary information. To ensure a smooth and efficient process, it is best to fill out the form completely before your appointment.
Documents used along the form
The Annual Physical Examination form is a crucial document that facilitates a comprehensive assessment of an individual's health. Alongside this form, several other documents may be utilized to ensure a thorough evaluation and record-keeping. Below is a list of these documents, each serving a unique purpose in the healthcare process.
- Medical History Form: This document collects detailed information about a patient's past medical history, including previous illnesses, surgeries, and family health history. It helps healthcare providers understand potential health risks and tailor their evaluations accordingly.
- Medication List: A comprehensive list of all medications the patient is currently taking, including over-the-counter drugs and supplements. This helps prevent potential drug interactions and ensures the provider has a complete picture of the patient's treatment regimen.
- Immunization Record: This record details the vaccinations the patient has received, including dates and types of immunizations. It is essential for assessing immunity and determining any necessary updates to vaccinations.
- Lab Test Results: Results from any recent laboratory tests, such as blood work or urinalysis, provide vital information about the patient's current health status. These results guide clinical decisions and treatment plans.
- Referral Forms: If a patient requires specialized care, referral forms document the need for consultation with other healthcare professionals. They ensure continuity of care and facilitate communication between providers.
- Consent Forms: These forms obtain patient consent for various procedures or treatments. They ensure that patients are informed about the risks and benefits of their healthcare options.
- Follow-Up Care Instructions: After the examination, patients may receive written instructions detailing recommended follow-up actions, including additional tests or lifestyle changes. This document helps patients understand their next steps in managing their health.
- Emergency Contact Form: This form lists individuals to be contacted in case of a medical emergency. It provides essential information to healthcare providers during urgent situations.
- Sales Tax Refund Affidavit: The ST-12B Georgia form is vital for individuals and businesses seeking to reclaim overpaid sales tax. To learn more about the process and access the form, visit georgiapdf.com/st-12b-georgia.
- Patient Satisfaction Survey: Often provided after a visit, this survey gathers feedback on the patient's experience with the healthcare provider. It helps improve services and address any concerns that patients may have.
These documents collectively contribute to a comprehensive approach to healthcare. They facilitate effective communication between patients and providers, ensuring that all aspects of a patient's health are considered and addressed appropriately.
Misconceptions
Understanding the Annual Physical Examination form is essential for ensuring a smooth medical appointment. However, several misconceptions may lead to confusion. Here are six common misconceptions explained:
- It is only for sick people. Many believe that an annual physical is only necessary if they are feeling unwell. In reality, these examinations are preventive measures that help identify potential health issues before they become serious.
- All information is optional. Some individuals think they can skip sections of the form. However, completing all requested information is crucial to avoid delays and ensure the healthcare provider has a complete picture of their health.
- Immunizations are not important. Some people underestimate the significance of immunizations listed on the form. Staying up-to-date with vaccinations is vital for preventing diseases and protecting overall health.
- Only new medications need to be listed. It is a common belief that only recent medications should be included. However, a complete list of all current medications, including over-the-counter drugs and supplements, is necessary for safe and effective care.
- Previous medical history is irrelevant. Many individuals think that their past health issues do not matter. In fact, a comprehensive medical history helps healthcare providers make informed decisions about current treatment and preventive measures.
- The form is the same for everyone. Some assume that the Annual Physical Examination form is standardized for all patients. Each person's health needs are unique, and the form may vary based on individual circumstances, age, and health conditions.
By addressing these misconceptions, individuals can better prepare for their annual physical examination and contribute to their overall health management.