Florida Do Not Resuscitate Order Document
In the state of Florida, the Do Not Resuscitate (DNR) Order form serves as a crucial document for individuals who wish to make their healthcare preferences clear, particularly in end-of-life situations. This form allows patients to communicate their desire to forgo cardiopulmonary resuscitation (CPR) in the event of a cardiac arrest or respiratory failure. By completing this form, individuals can ensure that their wishes are respected by medical professionals and family members during critical moments. The DNR Order must be signed by a physician, affirming that the patient is fully informed about their medical condition and the implications of the decision. Importantly, the form must be readily available and easily accessible, as emergency responders rely on it to guide their actions. Understanding the nuances of the DNR Order can empower individuals to make informed choices about their medical care, fostering peace of mind for both patients and their loved ones. This article will delve into the key components of the Florida DNR Order form, the process of obtaining one, and the significance of having such a directive in place.
Discover More Do Not Resuscitate Order Forms for Different States
Dnr Paper - A DNR order emphasizes a patient's quality of life over extended life through invasive procedures.
Dnrcc Meaning - Patients can use guidance from bioethics boards or counselors when considering a DNR.
When navigating the complexities of legal and financial responsibilities, securing a reliable Power of Attorney is essential. This important document ensures that your chosen representative can manage decisions on your behalf during unforeseen circumstances. For further assistance and resources related to these legal documents, you can visit All Ohio Forms, which provides valuable information and templates that cater to your specific needs.
Does a Dnr Need to Be Signed by a Doctor - It's advisable to review your DNR Order regularly to ensure it still aligns with your wishes.
Similar forms
- Advance Healthcare Directive: This document allows individuals to outline their preferences for medical treatment in case they become unable to communicate their wishes. It provides guidance on various healthcare decisions, similar to how a Do Not Resuscitate Order specifies preferences regarding resuscitation efforts.
- Living Will: A living will is a type of advance directive that details the types of medical treatment an individual wishes to receive or avoid at the end of life. Like the Do Not Resuscitate Order, it expresses a person's wishes concerning life-sustaining treatments.
- Durable Power of Attorney for Healthcare: This document designates a person to make healthcare decisions on behalf of an individual if they are unable to do so. It complements a Do Not Resuscitate Order by ensuring that someone can advocate for the individual's wishes regarding resuscitation and other medical interventions.
Employment Verification Form: This essential document confirms the employment status of individuals and is necessary for various processes. For those in Washington, the process is simplified by utilizing All Washington Forms to obtain the required verification swiftly.
- Physician Orders for Life-Sustaining Treatment (POLST): A POLST form translates a patient’s wishes about life-sustaining treatment into medical orders. It is similar to a Do Not Resuscitate Order, as it provides clear instructions for healthcare providers regarding the patient’s preferences.
- Do Not Intubate Order: This document specifically instructs healthcare providers not to use intubation to assist with breathing. It serves a similar purpose to a Do Not Resuscitate Order by outlining specific limitations on medical interventions.
- Comfort Care Order: A comfort care order focuses on providing relief from pain and distress rather than attempting to prolong life. It aligns with the principles of a Do Not Resuscitate Order by emphasizing quality of life over aggressive medical interventions.
- Healthcare Proxy: This document designates an individual to make healthcare decisions on behalf of someone else. It supports the intentions of a Do Not Resuscitate Order by ensuring that the appointed proxy can communicate and uphold the individual’s wishes regarding resuscitation.
- End-of-Life Care Plan: An end-of-life care plan outlines the type of care a person wishes to receive as they approach death. It is similar to a Do Not Resuscitate Order in that it expresses preferences for treatment and interventions during the final stages of life.
Document Example
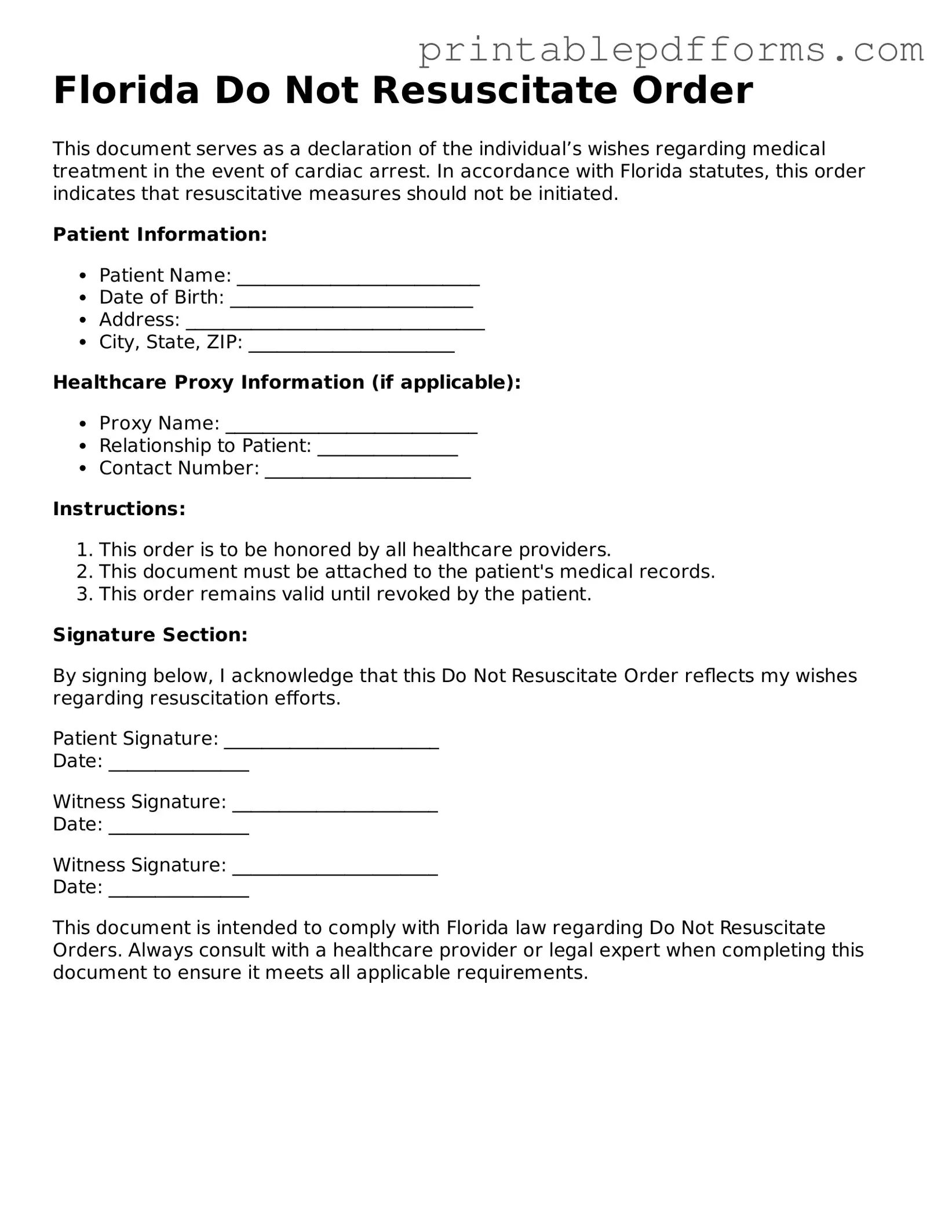
Florida Do Not Resuscitate Order
This document serves as a declaration of the individual’s wishes regarding medical treatment in the event of cardiac arrest. In accordance with Florida statutes, this order indicates that resuscitative measures should not be initiated.
Patient Information:
- Patient Name: __________________________
- Date of Birth: __________________________
- Address: ________________________________
- City, State, ZIP: ______________________
Healthcare Proxy Information (if applicable):
- Proxy Name: ___________________________
- Relationship to Patient: _______________
- Contact Number: ______________________
Instructions:
- This order is to be honored by all healthcare providers.
- This document must be attached to the patient's medical records.
- This order remains valid until revoked by the patient.
Signature Section:
By signing below, I acknowledge that this Do Not Resuscitate Order reflects my wishes regarding resuscitation efforts.
Patient Signature: _______________________
Date: _______________
Witness Signature: ______________________
Date: _______________
Witness Signature: ______________________
Date: _______________
This document is intended to comply with Florida law regarding Do Not Resuscitate Orders. Always consult with a healthcare provider or legal expert when completing this document to ensure it meets all applicable requirements.
PDF Form Specs
| Fact Name | Description |
|---|---|
| Definition | The Florida Do Not Resuscitate (DNR) Order form allows individuals to refuse resuscitation in the event of cardiac arrest or respiratory failure. |
| Governing Law | This form is governed by Florida Statutes, specifically Section 401.45, which outlines the requirements for DNR orders. |
| Eligibility | Any competent adult can complete a DNR order, or a legal guardian may do so on behalf of an incapacitated individual. |
| Signature Requirement | The form must be signed by the patient or their representative, as well as a physician to be valid. |
| Form Availability | The DNR order form is available online through the Florida Department of Health and can also be obtained from healthcare providers. |
| Revocation | A DNR order can be revoked at any time by the patient or their representative, either verbally or in writing. |
| Emergency Medical Services (EMS) Compliance | Emergency medical personnel are required to honor a valid DNR order, ensuring that the patient’s wishes are respected in emergencies. |
Crucial Questions on This Form
What is a Florida Do Not Resuscitate Order (DNRO)?
A Florida Do Not Resuscitate Order is a legal document that allows a person to refuse resuscitation in the event of a medical emergency. This means that if a person's heart stops beating or they stop breathing, medical personnel will not perform CPR or other life-saving measures. The DNRO is intended for individuals who have a terminal illness or a condition that significantly limits their quality of life.
Who can create a Do Not Resuscitate Order in Florida?
In Florida, any competent adult can create a DNRO. This includes individuals who are at least 18 years old and are capable of making their own healthcare decisions. Additionally, a parent or legal guardian can create a DNRO on behalf of a minor child. It is essential that the individual understands the implications of the order before signing it.
How is a Do Not Resuscitate Order completed?
To complete a DNRO in Florida, follow these steps:
- Obtain the official Florida DNRO form, which is available through healthcare providers or online.
- Fill out the form with the required personal information, including the individual's name and date of birth.
- Sign the form in the presence of a witness. The witness must also sign the document.
- Ensure that the DNRO is dated and that all sections are completed accurately.
Once the form is completed and signed, it should be kept in an easily accessible location, such as with other important medical documents.
Does a Do Not Resuscitate Order apply in all situations?
No, a DNRO specifically applies to situations where resuscitation is required, such as cardiac arrest or respiratory failure. It does not affect other medical treatments or interventions. For example, if a person is hospitalized for an unrelated condition, healthcare providers will still provide necessary medical care unless otherwise specified.
How can I ensure that my Do Not Resuscitate Order is honored?
To ensure that your DNRO is honored, consider the following steps:
- Keep a copy of the DNRO with you at all times, especially when visiting healthcare facilities.
- Inform family members, friends, and caregivers about your DNRO and its location.
- Discuss your wishes with your healthcare providers, so they are aware of your preferences.
- Consider wearing a medical alert bracelet that indicates the existence of a DNRO.
Can a Do Not Resuscitate Order be revoked?
Yes, a DNRO can be revoked at any time by the individual who created it. To revoke the order, simply destroy the original DNRO form and notify your healthcare providers and family members of the change. It is advisable to create a new document if you wish to express different healthcare preferences.
What should I do if I change my mind about my DNRO?
If you change your mind about your DNRO, you have the right to revoke it. Follow the steps mentioned earlier to revoke the order. Additionally, consider discussing your new wishes with your healthcare provider to ensure that your current preferences are clearly documented and understood.
Are there any costs associated with obtaining a Do Not Resuscitate Order?
In Florida, there is no fee for obtaining or completing a DNRO. However, some healthcare providers may charge for additional services related to discussing or documenting your healthcare preferences. It is always a good idea to check with your provider about any potential costs involved.
Where can I find more information about Do Not Resuscitate Orders in Florida?
For more information about DNROs in Florida, you can visit the Florida Department of Health website or contact your healthcare provider. They can provide guidance and resources to help you understand the process and implications of creating a Do Not Resuscitate Order.
Documents used along the form
When considering a Florida Do Not Resuscitate Order (DNRO), several other forms and documents can be important to ensure that your healthcare wishes are clear and respected. Below is a list of common documents that often accompany a DNRO, each serving a unique purpose.
- Advance Directive: This is a legal document that outlines your preferences for medical treatment in case you become unable to communicate your wishes. It can include instructions about life-sustaining treatments and appoint a healthcare proxy.
- Boat Bill of Sale: A legal document necessary for the transfer of boat ownership, ensuring proper recording of the transaction to protect both parties involved. More information can be found at nypdfforms.com/boat-bill-of-sale-form/.
- Healthcare Proxy: This document designates a specific person to make medical decisions on your behalf if you are unable to do so. It is essential for ensuring that someone you trust understands and can advocate for your healthcare preferences.
- Living Will: A living will details your wishes regarding medical treatment, particularly at the end of life. It can specify what types of interventions you do or do not want, providing guidance to healthcare providers and family members.
- Physician Orders for Life-Sustaining Treatment (POLST): This is a medical order that translates your treatment preferences into actionable orders for healthcare providers. It is often used for individuals with serious illnesses and complements the DNRO.
- Do Not Intubate (DNI) Order: This order specifically instructs healthcare providers not to insert a breathing tube if you are unable to breathe on your own. It is a separate directive that can be included in your overall treatment plan.
- Organ Donation Form: If you wish to donate your organs after death, this form allows you to express your intentions. It can be included with your DNRO to ensure that your wishes regarding organ donation are known.
- Patient Advocate Designation: This document allows you to appoint someone to advocate for your rights and preferences in a healthcare setting. It can be particularly useful in complex medical situations.
Having these documents in place can provide clarity and peace of mind regarding your healthcare decisions. They work together to ensure that your wishes are respected and that your loved ones and healthcare providers understand your preferences clearly.
Misconceptions
Understanding the Florida Do Not Resuscitate (DNR) Order form is crucial for making informed healthcare decisions. However, several misconceptions can cloud people's understanding. Here are six common myths about the DNR form:
- A DNR means no medical care at all. Many believe that having a DNR order means that a patient will receive no medical treatment. In reality, a DNR only pertains to resuscitation efforts during cardiac arrest. Other medical treatments can still be provided.
- Only terminally ill patients need a DNR. Some think DNR orders are only for those who are terminally ill. However, anyone can choose a DNR based on their personal health wishes, regardless of their current health status.
- A DNR is a legally binding document everywhere. While the DNR is recognized in Florida, it may not hold the same weight in other states. It's important to understand local laws if traveling or relocating.
- Once signed, a DNR cannot be changed. Many people assume that a DNR order is permanent and cannot be altered. In fact, individuals can revoke or modify their DNR at any time, as long as they are mentally competent to do so.
- Healthcare providers will ignore a DNR order. Some fear that medical professionals may not honor a DNR. However, healthcare providers are trained to respect DNR orders and will follow the patient's wishes as outlined in the document.
- A DNR order is the same as a living will. While both documents relate to end-of-life care, they serve different purposes. A living will outlines a person's wishes regarding medical treatment in various scenarios, whereas a DNR specifically addresses resuscitation efforts.
By debunking these misconceptions, individuals can make more informed choices regarding their healthcare preferences and ensure that their wishes are respected.