Fill a Valid Medication Administration Record Sheet Form
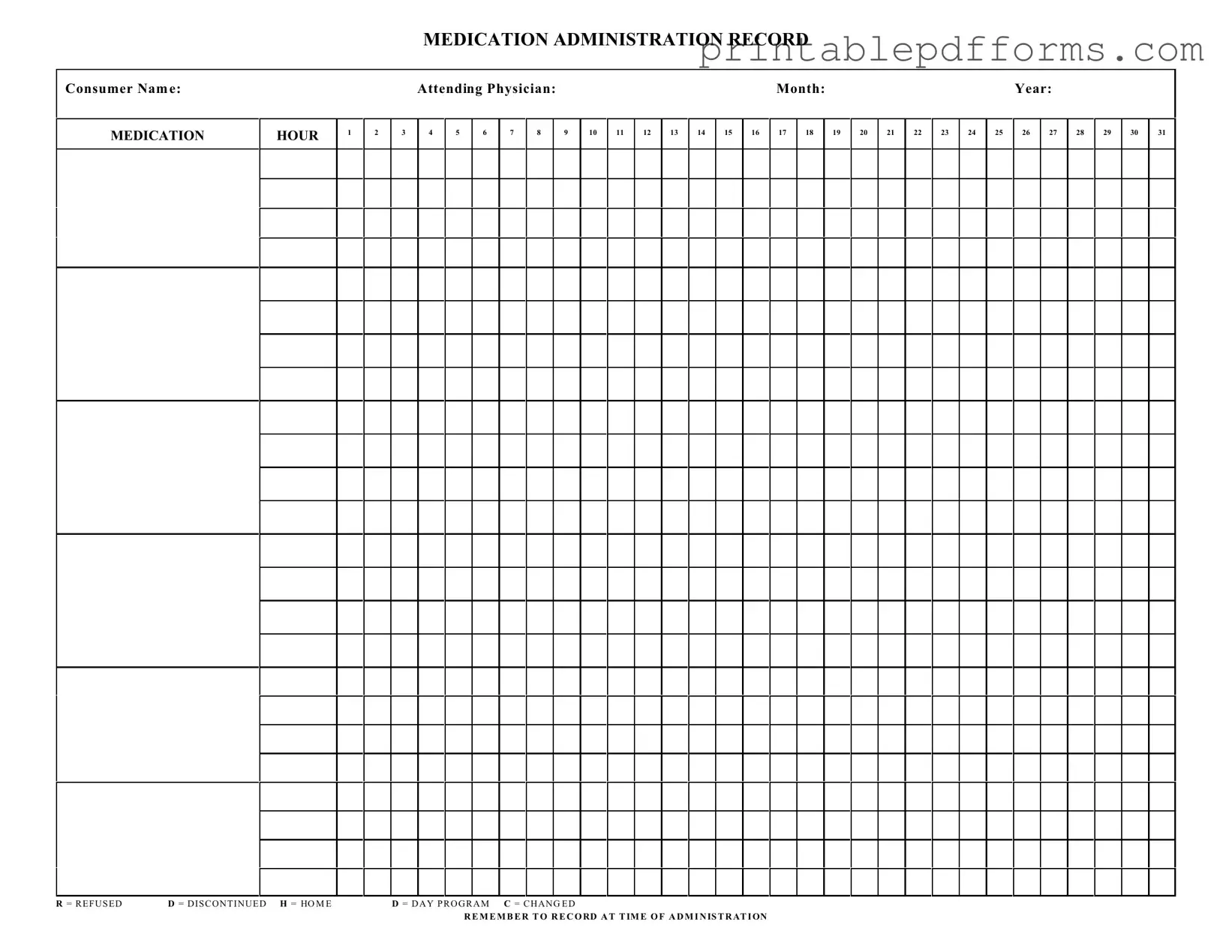
The Medication Administration Record Sheet (MARS) is an essential tool in healthcare settings, ensuring that patients receive their medications accurately and on time. This form captures vital information, including the consumer's name, the attending physician, and the specific month and year of medication administration. It provides a structured layout for recording medication dosages at various hours throughout the day. Each hour is designated with a corresponding box where healthcare providers can document the administration status. Options such as "Refused," "Discontinued," "Home," "Day Program," and "Changed" allow for clear communication regarding any alterations in medication delivery. It is crucial for caregivers to remember to record the administration at the exact time it occurs, maintaining an accurate and comprehensive record. This attention to detail not only supports patient safety but also facilitates effective communication among the healthcare team.
Additional PDF Templates
Aia A305 Form Pdf - This form can be a tool for evaluating a contractor's stability.
Prescription Form - Physicians find the Prescription Pad indispensable for managing patient medication regimens effectively.
The WC-200A Georgia form is a crucial document used to request a change of physician or additional treatment in workers' compensation cases. Properly filling out this form is essential for ensuring that employees receive the medical care they need while also complying with state regulations. For more information, you can refer to the official resource at https://georgiapdf.com/wc-200a-georgia/. Take action now to ensure your rights are protected by filling out the form below.
T-47 - It is important for confirming the seller's authority to sell the residential property.
Similar forms
The Medication Administration Record Sheet form shares similarities with several other important documents used in healthcare settings. Each of these documents serves a unique purpose while also maintaining a focus on patient care and medication management. Below is a list of documents that are comparable to the Medication Administration Record Sheet form:
- Patient Medication List: This document provides a comprehensive overview of all medications a patient is currently taking. Like the Medication Administration Record Sheet, it ensures that healthcare providers have accurate information to prevent medication errors.
- Medication Reconciliation Form: This form is used during transitions of care, such as hospital admissions or discharges. It helps verify that a patient's medication list is accurate and complete, similar to how the Medication Administration Record Sheet tracks administration details.
- Nursing Notes: Nursing notes document patient observations and care provided. They often include medication administration details, paralleling the Medication Administration Record Sheet in terms of tracking patient care over time.
- Notice to Quit Form: The Ohio Notice to Quit form is crucial for landlords, providing a formal notification to tenants about lease violations. For more information, visit All Ohio Forms.
- Pharmacy Dispensing Record: This record outlines the medications dispensed by a pharmacy. It aligns with the Medication Administration Record Sheet by ensuring that the right medications are provided to patients and that proper documentation is maintained.
- Care Plan: A care plan outlines the overall treatment strategy for a patient, including medication management. It is similar to the Medication Administration Record Sheet in that both documents focus on the patient's health and medication needs.
- Incident Report: This document is used to report any medication errors or adverse events. While it serves a different purpose, it relates to the Medication Administration Record Sheet by highlighting the importance of accurate medication administration and patient safety.
Document Example
MEDICATION ADMINISTRATION RECORD
Consumer Nam e:
MEDICATION
HOUR
1
2
|
Attending Physician: |
|
|
|
|
|
|
|
|
Month: |
|
|
|
|
|
|
|
Year: |
|
|
|
|
||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
3 |
4 |
5 |
6 |
7 |
8 |
|
9 |
10 |
11 |
12 |
13 |
14 |
15 |
16 |
17 |
18 |
|
19 |
20 |
21 |
22 |
23 |
24 |
25 |
26 |
27 |
28 |
29 |
30 |
31 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
R = R E F U S E D |
D = D I S C O N T I N U E D H = HO M E |
D = D A Y P R O G R A M C = C H A N G E D |
R E M E M B E R T O R E C O RD A T T IM E O F A D M I N IS T R AT I ON
Form Specs
| Fact Name | Description |
|---|---|
| Purpose | The Medication Administration Record (MAR) is used to track the administration of medications to consumers. |
| Consumer Information | Each MAR includes essential details such as the consumer's name and the attending physician's name. |
| Monthly Tracking | The form allows for daily tracking of medication administration throughout each month, covering all 31 days. |
| Administration Codes | Common codes like R (Refused), D (Discontinued), and H (Home) help indicate the status of medication administration. |
| State Regulations | In some states, the use of MARs is governed by specific laws, such as the Nurse Practice Act or state pharmacy regulations. |
| Documentation Requirement | It is crucial to record the administration of medications at the time they are given to ensure accurate documentation. |
Crucial Questions on This Form
What is the purpose of the Medication Administration Record Sheet?
The Medication Administration Record Sheet is designed to track the administration of medications to consumers. It helps ensure that medications are given at the correct times and in the appropriate doses, enhancing patient safety and compliance with treatment plans.
How do I fill out the Medication Administration Record Sheet?
To fill out the form, start by entering the consumer's name and the attending physician's name at the top. Then, for each day of the month, record the medications administered at the designated hours. Use the codes provided (R, D, H, C) to indicate any refusals, discontinuations, home medications, or changes in medication.
What do the abbreviations R, D, H, and C stand for?
These abbreviations are used to indicate the status of medication administration:
- R = Refused
- D = Discontinued
- H = Home medication
- C = Changed
Why is it important to record the time of administration?
Recording the time of administration is crucial for several reasons. It ensures that medications are given consistently and helps healthcare providers monitor the effectiveness of the treatment. It also provides a clear record for any future evaluations or adjustments needed in the medication regimen.
Can I use the Medication Administration Record Sheet for multiple consumers?
No, the Medication Administration Record Sheet is intended for individual consumers only. Each consumer should have their own record to maintain accurate and personalized medication tracking.
What should I do if a consumer refuses their medication?
If a consumer refuses their medication, mark the appropriate box with an "R" on the record sheet. It’s also important to document any reasons for refusal and notify the attending physician or relevant healthcare team members to ensure proper follow-up.
How often should I update the Medication Administration Record Sheet?
The record sheet should be updated daily, or each time medication is administered. This ensures that the information is current and accurately reflects the consumer's medication history.
What if there is a change in the medication prescribed?
If there is a change in the medication, mark the appropriate box with a "C" and update the medication details on the record sheet. It’s essential to communicate these changes to all relevant healthcare team members to maintain continuity of care.
Who is responsible for maintaining the Medication Administration Record Sheet?
The responsibility for maintaining the Medication Administration Record Sheet typically falls on the healthcare provider administering the medication. However, all team members involved in the consumer's care should be aware of the information recorded to ensure a coordinated approach to treatment.
Documents used along the form
The Medication Administration Record Sheet is an essential document used in healthcare settings to track the administration of medications to patients. Alongside this form, several other documents are commonly utilized to ensure proper medication management and patient care. Below is a list of related forms and documents that may accompany the Medication Administration Record Sheet.
- Patient Medication Profile: This document provides a comprehensive overview of a patient's medication history, including current prescriptions, dosages, and any known allergies. It helps healthcare providers make informed decisions regarding medication administration.
- Medication Order Form: This form is used by physicians to prescribe medications for patients. It includes details such as the medication name, dosage, route of administration, and frequency. This form is crucial for ensuring that the correct medications are given to the right patients.
- Medication Reconciliation Form: This document is used to compare a patient's current medications with those being prescribed during a transition of care. It aims to prevent medication errors and ensure continuity of care by identifying discrepancies.
- Incident Report Form: In case of any adverse reactions or medication errors, this form is completed to document the incident. It includes details about the event, actions taken, and any follow-up measures necessary to improve patient safety.
- Motor Vehicle Bill of Sale: This important document records the sale of a motor vehicle in Texas, capturing essential details about the transaction. For more information, visit https://freebusinessforms.org.
- Patient Consent Form: Before administering certain medications, especially those with significant risks, healthcare providers may require patients to sign a consent form. This document ensures that patients are informed about the treatment and agree to proceed.
These documents work together to promote safe and effective medication administration. Proper use of these forms can significantly enhance patient care and minimize the risk of medication-related issues.
Misconceptions
Understanding the Medication Administration Record Sheet (MARS) is essential for ensuring accurate medication management. However, several misconceptions exist that can lead to confusion. Below are ten common misconceptions, along with clarifications to help you better understand this important document.
- Misconception 1: The MARS is only for nurses.
- Misconception 2: It is unnecessary to document refused medications.
- Misconception 3: The MARS is only relevant for long-term care facilities.
- Misconception 4: Any errors in the MARS can be easily corrected later.
- Misconception 5: The MARS only tracks medication schedules.
- Misconception 6: It is acceptable to skip recording a dose if it was not administered.
- Misconception 7: Only one person can fill out the MARS.
- Misconception 8: The MARS does not need to be reviewed regularly.
- Misconception 9: The MARS is a legal document and cannot be altered.
- Misconception 10: The MARS is only for prescription medications.
This form is used by various healthcare providers, including caregivers and family members, to track medication administration for individuals receiving care.
Documenting refused medications is crucial. It provides a complete picture of the patient's medication history and helps inform future care decisions.
The MARS can be used in various settings, including home care, day programs, and hospitals. Its versatility makes it applicable across different healthcare environments.
While mistakes can sometimes be amended, it is essential to document them accurately at the time of administration. This ensures that all parties involved have access to the correct information.
In addition to medication schedules, the MARS also records important notes about medication changes, refusals, and other relevant patient information.
Every dose, whether administered or not, should be recorded. This practice helps maintain a clear and accurate medication history.
Multiple caregivers can contribute to the MARS, as long as they are properly trained and understand the importance of accurate documentation.
Regular reviews of the MARS are necessary to ensure that all entries are accurate and up-to-date. This practice helps identify any discrepancies or issues that may arise.
While the MARS serves as a record of medication administration, it can be corrected with appropriate documentation of errors, such as initialing and dating the changes.
In fact, the MARS can also be used to track over-the-counter medications and supplements, ensuring comprehensive medication management.
By addressing these misconceptions, you can enhance your understanding of the Medication Administration Record Sheet and its importance in providing safe and effective care.