Fill a Valid Tb Test Form
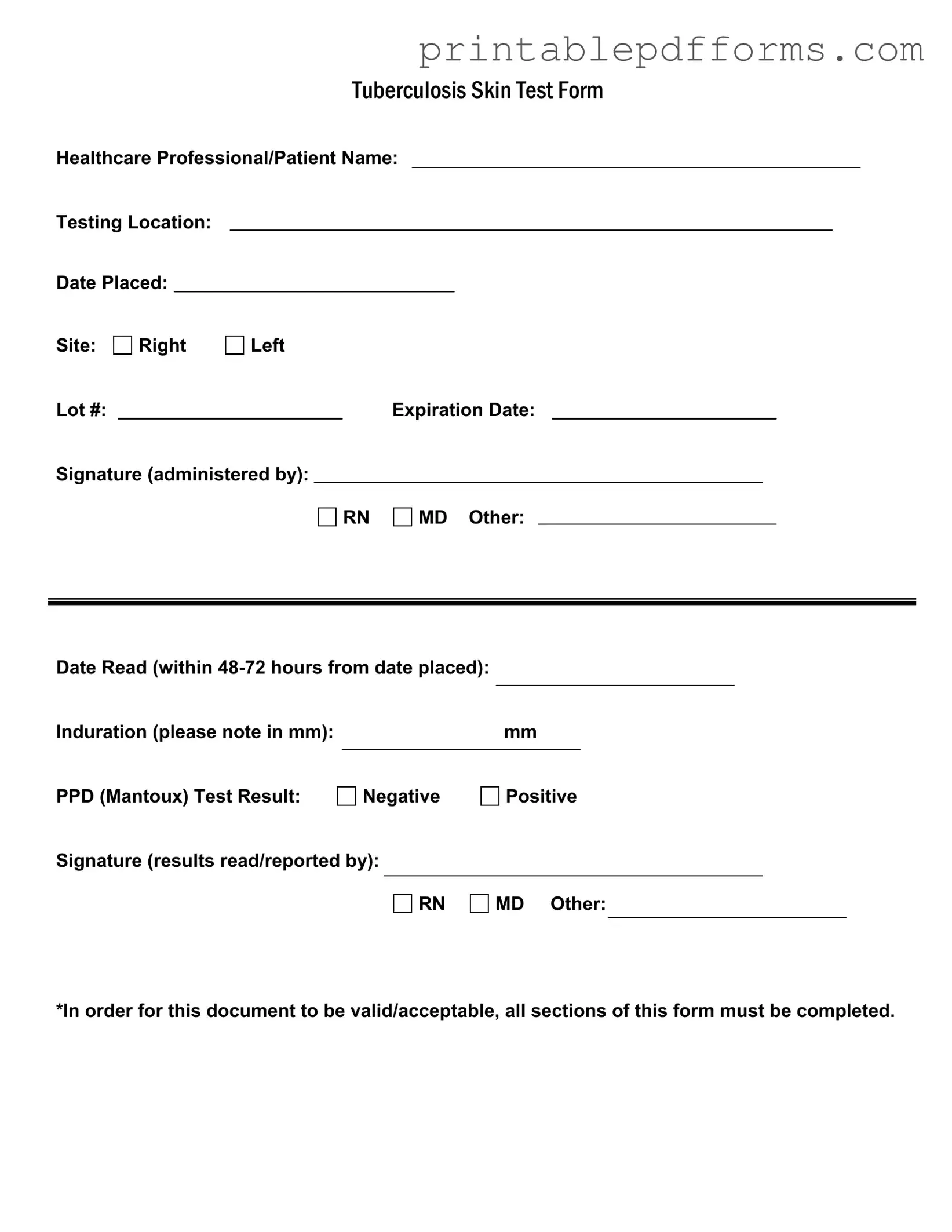
The Tuberculosis (TB) Test form is a crucial document used in the healthcare sector to record essential information regarding the administration and results of the TB skin test, commonly known as the PPD (Purified Protein Derivative) test. This form captures key details such as the names of both the healthcare professional and the patient, along with the location where the test was conducted. It specifies the date the test was placed and the site of administration, whether on the right or left arm. Additionally, the form includes important identifiers like the lot number of the test and its expiration date, ensuring that the test is both valid and reliable. After the test is administered, the healthcare provider must sign the form, confirming their role in the process. The results, which must be read within 48 to 72 hours, indicate the degree of induration measured in millimeters, ultimately determining whether the test result is negative or positive. A signature from the healthcare professional who reads and reports the results is also required. It is vital that all sections of this form are completed to ensure its validity and acceptance in medical records and public health reporting.
Additional PDF Templates
How to Obtain My College Transcripts - Include the date you are making the request on the form.
The Ohio Payoff Form is crucial for facilitating debt resolution in property transactions, serving as a key document that realtors and title companies utilize to obtain necessary payoff information. This form, administered by the Collections Enforcement Section under the Attorney General of Ohio, requires consent from individuals or entities to release information on certified debts and liens, ensuring a transparent process. For more information on related processes and documentation, you can refer to All Ohio Forms, which offers resources to streamline these procedures efficiently.
Da - Provides essential data for inventory reconciliation.
Similar forms
Vaccination Record: Similar to the TB Test form, a vaccination record includes patient information, the date of vaccination, and the healthcare professional's signature. Both documents serve as proof of medical interventions.
Medical History Form: This form collects patient information regarding past illnesses, treatments, and allergies. Like the TB Test form, it requires completion of all sections to be valid.
Consent Form: A consent form outlines the procedures and risks associated with a medical test or treatment. It shares the requirement for signatures from both the patient and the healthcare provider, ensuring informed consent.
Patient Assessment Form: This document records a patient's health status and symptoms. Similar to the TB Test form, it is critical for diagnosis and requires thorough completion by the healthcare provider.
Referral Form: A referral form facilitates the transfer of patient information between healthcare providers. It parallels the TB Test form in its need for detailed patient data and signatures to validate the referral.
Laboratory Test Requisition: This form requests specific laboratory tests and includes patient details, similar to the TB Test form. Both require accurate completion to ensure proper testing and results reporting.
Divorce Settlement Agreement: This crucial document specifies the terms of a divorce, detailing asset division, child support, and alimony. For assistance in obtaining this form, visit All Washington Forms.
Follow-Up Appointment Notice: This document schedules a follow-up visit and includes patient information and dates. Like the TB Test form, it requires clarity and completeness to ensure proper patient care.
Document Example
|
|
|
|
|
TUBERCULOSISSKINTESTFORM |
||||||||
Healthcare Professional/Patient Name: |
|||||||||||||
Testing Location: |
|
|
|
|
|
|
|
|
|
|
|
||
Date Placed: |
|
|
|
|
|
|
|
|
|
|
|
|
|
Site: |
Right |
Left |
|
|
|
|
|
|
|
|
|||
Lot #: |
|
|
|
|
|
Expiration Date: |
|
|
|||||
Signature (administered by): |
|
|
|
|
|
|
|
|
|
||||
|
|
|
|
|
RN |
|
MD Other: |
|
|
|
|||
Date Read (within |
|
|
|
|
|
|
|
Induration (please note in mm): |
|
mm |
|
PPD (Mantoux) Test Result: |
|
|
|
Negative |
Positive |
||
Signature (results read/reported by):
RN
MD Other:
*In order for this document to be valid/acceptable, all sections of this form must be completed.
Form Specs
| Fact Name | Description |
|---|---|
| Healthcare Professional Information | The form requires the name of the healthcare professional administering the test, ensuring accountability and proper documentation. |
| Testing Location | The specific location where the test is conducted must be recorded, providing clarity on where the procedure took place. |
| Date and Site of Test | Both the date the test was placed and the site (right or left arm) must be noted. This information is crucial for tracking and follow-up. |
| Induration Measurement | Induration, measured in millimeters, must be documented within 48-72 hours after placement. This measurement is essential for interpreting the test results. |
| Signature Requirement | The form must include signatures from both the administering healthcare professional and the individual reading the results. This ensures that all steps of the testing process are verified. |
Crucial Questions on This Form
What is the purpose of the TB Test form?
The TB Test form is used to document the administration and results of the Tuberculosis (TB) skin test, also known as the PPD (Purified Protein Derivative) test. This form captures essential information such as the patient's name, the testing location, and the date the test was placed and read. Proper completion of this form is crucial for ensuring that the test results are valid and can be used for medical or employment purposes.
What information must be included on the TB Test form?
To ensure the TB Test form is valid, all sections must be completed. Key information includes:
- Healthcare professional or patient name
- Testing location
- Date the test was placed
- Site of administration (right or left arm)
- Lot number and expiration date of the PPD solution
- Signature of the healthcare professional who administered the test
- Date the test results were read (within 48-72 hours)
- Induration measurement in millimeters
- Result of the test (negative or positive)
- Signature of the healthcare professional who read the results
Completing all these sections ensures that the form is accepted by employers, schools, or healthcare facilities.
How soon should the TB test results be read?
The TB test results should be read within 48 to 72 hours after the test is administered. This timeframe is critical because it allows for an accurate measurement of induration, which is the raised area that indicates a reaction to the test. If the results are not read within this window, the test may need to be repeated.
What do the results of the TB test mean?
The TB test results can be either negative or positive:
- Negative Result: This means that there was no significant reaction to the test, suggesting that the person likely does not have a TB infection.
- Positive Result: This indicates that there was a significant reaction, which may suggest a TB infection. However, it does not confirm active TB disease. Further testing, such as a chest X-ray or a sputum test, may be required to determine if the person has active TB.
It is important to discuss any positive results with a healthcare professional for appropriate follow-up and treatment options.
Documents used along the form
The Tuberculosis (TB) Test form is an essential document used in healthcare settings to record the administration and results of a TB skin test. However, it is often accompanied by several other forms and documents that support the testing process and ensure proper patient management. Below is a list of related documents that may be used alongside the TB Test form.
- Patient Consent Form: This document ensures that the patient understands the procedure and gives their permission for the TB test to be performed. It outlines any potential risks and benefits associated with the test.
- WC-240 Form: This critical document informs employees about job offers suitable for their health conditions, enhancing their ability to return to work effectively. For more information, visit georgiapdf.com/wc-240-georgia.
- Health History Questionnaire: A form that collects information about the patient’s medical history, including any previous TB exposure, existing health conditions, and current medications. This helps healthcare providers assess the patient's risk factors.
- Referral Form: Used when a patient needs to be referred to a specialist or a different healthcare facility for further evaluation or treatment related to TB. This form includes essential patient information and the reason for referral.
- Follow-Up Appointment Schedule: A document that outlines the timeline for follow-up appointments after the TB test is administered. It ensures that patients return for the reading of the test results and any necessary further action.
- TB Screening Questionnaire: This form is often used to assess symptoms related to TB, such as cough, fever, or weight loss. It helps healthcare providers determine if additional testing or treatment is needed.
- Results Notification Form: A document that communicates the results of the TB test to the patient. It may include information on what the results mean and any recommended next steps based on the findings.
- Immunization Record: This record tracks the patient’s vaccination history, which can be relevant in evaluating their overall health and risk for TB. It may also include information about other vaccinations that are important for public health.
Each of these documents plays a crucial role in the TB testing process, ensuring that patients receive comprehensive care and follow-up as needed. Proper documentation helps healthcare providers make informed decisions about patient health and safety.
Misconceptions
Understanding the Tuberculosis (TB) test form is essential for both healthcare professionals and patients. However, several misconceptions can lead to confusion. Here are eight common misunderstandings:
- The form is optional. Many people believe that completing the TB test form is optional. In reality, all sections must be filled out for the document to be valid.
- Any healthcare professional can administer the test. While various professionals can administer the test, it is crucial that the person is qualified, such as a registered nurse (RN) or a medical doctor (MD).
- Results can be read anytime after the test is placed. Some individuals think they can check the results at their convenience. However, the results must be read within 48 to 72 hours of placement for accuracy.
- A positive result always means active TB. A common misconception is that a positive result indicates active tuberculosis. In fact, it may simply indicate past exposure or infection.
- Induration size is irrelevant. Some believe that the size of the induration (swelling) does not matter. However, the measurement in millimeters is critical for interpreting the test results.
- The expiration date is not important. Many overlook the expiration date of the PPD (Purified Protein Derivative) used in the test. Using expired materials can lead to inaccurate results.
- Only one signature is needed on the form. Some think that only the administering professional needs to sign the form. In reality, both the person administering the test and the one reading the results must provide their signatures.
- All TB tests are the same. There is a belief that all TB tests are identical. However, the Mantoux test is specific and requires a particular process that differs from other TB testing methods.
Clarifying these misconceptions can help ensure that TB testing is performed correctly and that individuals receive accurate information regarding their health.