Texas Do Not Resuscitate Order Document
In Texas, the Do Not Resuscitate (DNR) Order form serves as a vital tool for individuals wishing to communicate their preferences regarding medical treatment in critical situations. This legally recognized document allows patients to express their desire to forgo resuscitation efforts in the event of cardiac arrest or respiratory failure. It is essential for ensuring that healthcare providers respect the wishes of patients and their families during some of the most challenging moments. The DNR Order includes key components, such as the patient’s name, date of birth, and signature, as well as the signatures of the attending physician and a witness. Importantly, the form must be completed with careful consideration, as it reflects deeply personal choices about end-of-life care. Understanding the implications of a DNR Order can empower individuals to make informed decisions about their healthcare, while also providing peace of mind to loved ones. In this article, we will explore the intricacies of the Texas DNR Order form, its legal significance, and the steps involved in obtaining and implementing it effectively.
Discover More Do Not Resuscitate Order Forms for Different States
Dnr Paper - Family members should be informed about the existence of a DNR order to ensure they understand the patient's wishes.
Completing the Washington Divorce Settlement Agreement form can be a daunting task, yet it is essential for clarifying each party's responsibilities and rights after the divorce. To facilitate this process, we encourage you to explore All Washington Forms that can provide guidance and resources to ensure that your agreement is comprehensive and fair.
Dnrcc Meaning - This document specifies that no CPR or advanced life-saving procedures should be performed.
Do Not Resuscitate Form Florida - A DNR does not limit other forms of medical care; it only addresses resuscitation efforts.
Where to Get a Dnr - Often part of a broader advance care planning conversation.
Similar forms
A Do Not Resuscitate (DNR) Order is a crucial document in healthcare, indicating a patient's wish not to receive cardiopulmonary resuscitation (CPR) in the event of cardiac arrest. Several other documents serve similar purposes in outlining a person's medical preferences. Here’s a look at nine documents that share similarities with a DNR Order:
- Advance Healthcare Directive: This document allows individuals to specify their healthcare preferences, including decisions about life-sustaining treatments, much like a DNR.
- Living Will: A living will details the types of medical treatment a person wishes to receive or avoid, particularly in terminal situations, paralleling the intent of a DNR.
- Durable Power of Attorney for Healthcare: This document designates a trusted individual to make healthcare decisions on behalf of a person, similar to how a DNR communicates specific wishes.
- Physician Orders for Life-Sustaining Treatment (POLST): POLST forms translate a patient's wishes into actionable medical orders, encompassing DNR preferences and other treatment choices.
- Do Not Intubate (DNI) Order: A DNI order specifically states that a patient does not wish to be intubated, focusing on breathing assistance, akin to the resuscitation limitations of a DNR.
- Comfort Care Order: This document emphasizes the provision of comfort measures rather than aggressive treatment, aligning with the goals of a DNR to avoid unnecessary interventions.
- End-of-Life Care Plan: An end-of-life care plan outlines a person’s wishes for their final days, including preferences for resuscitation, similar to a DNR's intent.
Articles of Incorporation: This essential document serves as the foundation for establishing a corporation in New York. Properly completing and filing the nypdfforms.com/articles-of-incorporation-form/ is vital for anyone looking to launch a business in the state.
- Medical Orders for Scope of Treatment (MOST): This document provides detailed instructions regarding the scope of treatment a patient desires, including resuscitation status, paralleling the DNR.
- Patient Preferences for Resuscitation: This informal document can be used to communicate a patient’s wishes regarding resuscitation efforts, serving a purpose similar to that of a DNR order.
Understanding these documents can empower individuals to make informed decisions about their healthcare preferences, ensuring that their wishes are respected in critical situations.
Document Example
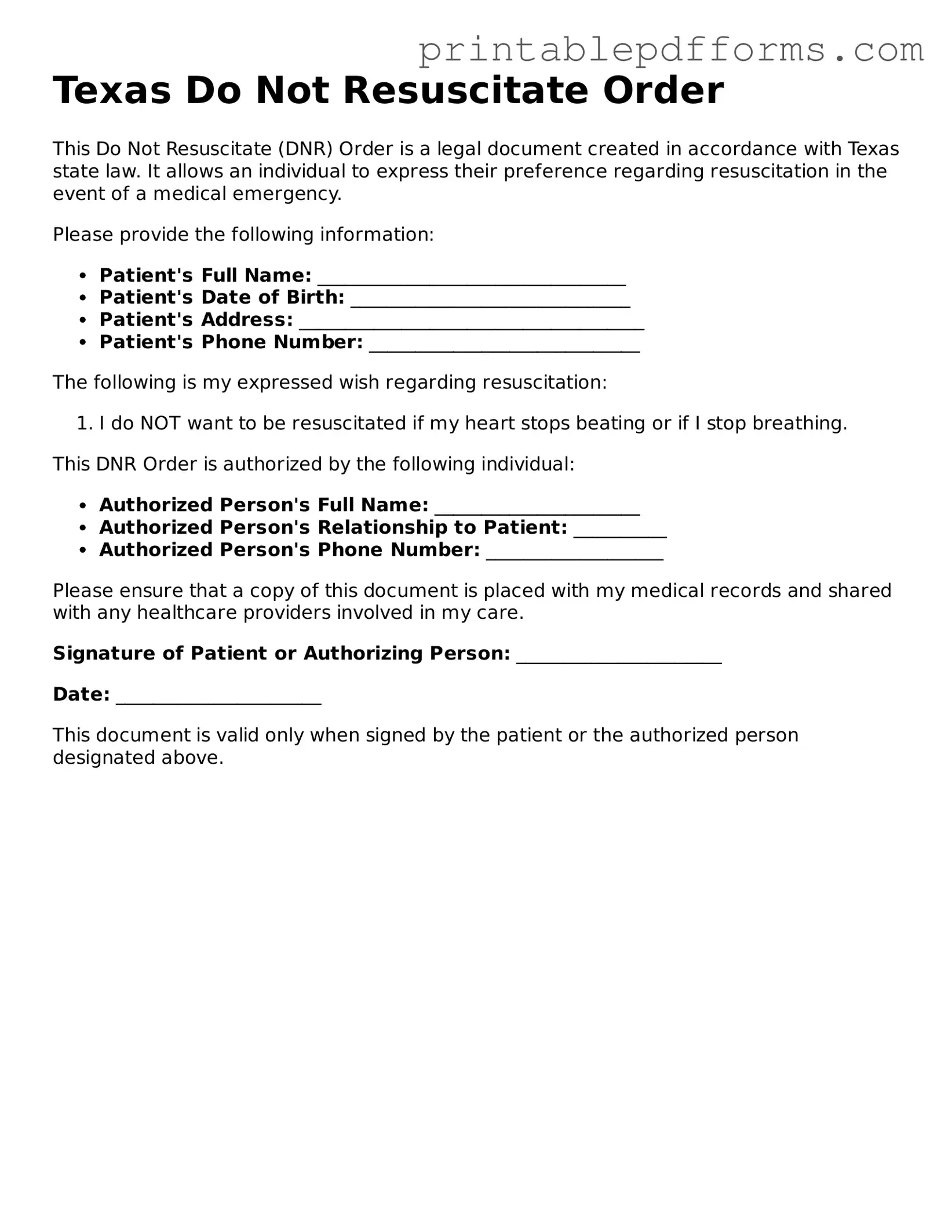
Texas Do Not Resuscitate Order
This Do Not Resuscitate (DNR) Order is a legal document created in accordance with Texas state law. It allows an individual to express their preference regarding resuscitation in the event of a medical emergency.
Please provide the following information:
- Patient's Full Name: _________________________________
- Patient's Date of Birth: ______________________________
- Patient's Address: _____________________________________
- Patient's Phone Number: _____________________________
The following is my expressed wish regarding resuscitation:
- I do NOT want to be resuscitated if my heart stops beating or if I stop breathing.
This DNR Order is authorized by the following individual:
- Authorized Person's Full Name: ______________________
- Authorized Person's Relationship to Patient: __________
- Authorized Person's Phone Number: ___________________
Please ensure that a copy of this document is placed with my medical records and shared with any healthcare providers involved in my care.
Signature of Patient or Authorizing Person: ______________________
Date: ______________________
This document is valid only when signed by the patient or the authorized person designated above.
PDF Form Specs
| Fact Name | Description |
|---|---|
| Definition | The Texas Do Not Resuscitate (DNR) Order is a legal document that allows a person to refuse resuscitation in the event of cardiac or respiratory arrest. |
| Governing Law | The Texas DNR Order is governed by the Texas Health and Safety Code, specifically Chapter 166. |
| Eligibility | Any adult who is competent to make medical decisions can execute a DNR order, or a legally authorized representative can do so on behalf of a patient. |
| Form Requirements | The DNR order must be in writing and signed by the patient or their representative, along with the physician's signature. |
| Validity | The Texas DNR Order remains valid across different healthcare settings, including hospitals, nursing homes, and home care. |
| Revocation | A DNR order can be revoked at any time by the patient or their representative, either verbally or in writing. |
| Emergency Medical Services | Emergency medical services (EMS) personnel are required to honor a valid DNR order when they encounter a patient in cardiac or respiratory arrest. |
Crucial Questions on This Form
What is a Texas Do Not Resuscitate Order (DNR)?
A Texas Do Not Resuscitate Order (DNR) is a legal document that allows individuals to express their wishes regarding resuscitation efforts in the event of a medical emergency. If a person is unable to communicate their preferences, this order guides healthcare providers on whether or not to perform cardiopulmonary resuscitation (CPR) and other life-saving measures.
Who can request a DNR in Texas?
In Texas, a DNR can be requested by a competent adult or a legal guardian. Additionally, a person’s healthcare proxy or agent, designated under a medical power of attorney, may also request a DNR on behalf of the individual if they are unable to do so.
How do I obtain a DNR form in Texas?
You can obtain a Texas DNR form from various sources, including:
- Healthcare providers, such as hospitals or clinics.
- State health department websites.
- Online resources that provide legal documents related to healthcare.
It’s important to ensure that the form is the official Texas DNR form to ensure its validity.
What information is required on the DNR form?
The Texas DNR form typically requires the following information:
- The name and date of birth of the individual.
- The signature of the individual or their legal representative.
- The date the form was signed.
- Contact information for the person completing the form.
In some cases, a physician’s signature may also be required to validate the order.
Is a DNR order valid in all healthcare settings?
Yes, a DNR order is generally valid across all healthcare settings in Texas, including hospitals, nursing homes, and emergency medical services. However, it’s crucial to ensure that the order is easily accessible and clearly visible to healthcare providers at all times.
Can a DNR order be revoked?
Absolutely. A DNR order can be revoked at any time by the individual or their legal representative. To revoke the order, simply destroy the original document and inform healthcare providers of the change in wishes. It’s advisable to complete a new DNR form if you wish to establish a different set of instructions.
What happens if I don’t have a DNR order?
If a person does not have a DNR order and experiences a medical emergency, healthcare providers are required to perform resuscitation efforts, including CPR. This can lead to unwanted medical interventions, particularly for individuals who may not wish to receive them.
Can I discuss my DNR wishes with my family?
Yes, discussing your DNR wishes with family members is highly encouraged. Open conversations can help ensure that your loved ones understand your preferences and can advocate for them if necessary. It can also reduce confusion or conflict during critical moments.
Are there any costs associated with obtaining a DNR order?
Generally, there are no costs associated with obtaining a Texas DNR order itself. However, some healthcare providers may charge for the services related to discussing and documenting your wishes. Always check with your healthcare provider for any potential fees.
Documents used along the form
The Texas Do Not Resuscitate (DNR) Order form is an important document that allows individuals to express their wishes regarding resuscitation efforts in the event of a medical emergency. Alongside this form, several other documents often play a crucial role in ensuring that a person's healthcare preferences are honored. Below is a list of these related forms and documents.
- Advance Directive: This document outlines a person's wishes regarding medical treatment and care if they become unable to communicate those wishes themselves. It can include preferences for life-sustaining treatments and appoint a healthcare proxy.
- Medical Power of Attorney: This legal document allows a person to designate someone else to make healthcare decisions on their behalf if they are incapacitated. It is vital for ensuring that a trusted individual can advocate for the patient's preferences.
- Living Will: A living will specifies what types of medical treatment an individual wishes to receive or avoid in certain situations, particularly when facing terminal illness or irreversible conditions.
- Physician Orders for Life-Sustaining Treatment (POLST): This form translates a patient’s preferences regarding life-sustaining treatment into actionable medical orders. It is often used for patients with serious illnesses or those nearing the end of life.
- Ohio Payoff Form: This form is essential for realtors and title companies to request payoff information regarding debts owed to the State of Ohio. All Ohio Forms can be used to access this important document, ensuring clarity and efficiency in debt resolution.
- Do Not Intubate (DNI) Order: This document specifies that a patient should not be placed on a ventilator if they experience respiratory failure. It is often used in conjunction with DNR orders.
- Healthcare Proxy: Similar to a medical power of attorney, a healthcare proxy designates an individual to make medical decisions on behalf of the patient. This document can work alongside advance directives to clarify the patient's wishes.
- Comfort Care Order: This order focuses on providing comfort measures rather than curative treatment. It ensures that patients receive palliative care that prioritizes their comfort and quality of life.
- Emergency Medical Services (EMS) DNR Form: This form is specifically for emergency medical services personnel. It informs them of a patient’s DNR status and ensures that the patient's wishes are respected in emergency situations.
Understanding these documents is essential for individuals who wish to ensure their healthcare preferences are respected. Each document serves a specific purpose and can work together to create a comprehensive plan for medical care in accordance with a person's wishes.
Misconceptions
Understanding the Texas Do Not Resuscitate (DNR) Order form is essential for individuals and families making important healthcare decisions. However, several misconceptions can lead to confusion. Here are nine common misunderstandings about the Texas DNR Order form:
-
A DNR means no medical care will be provided.
This is not true. A DNR specifically addresses resuscitation efforts in the event of cardiac arrest. Other medical treatments and interventions can still be administered as needed.
-
A DNR is only for terminally ill patients.
While many people associate DNRs with terminal illness, anyone can have a DNR, regardless of their health status. It’s a personal choice based on individual values and preferences.
-
A DNR is permanent and cannot be changed.
This misconception is incorrect. Individuals can revoke or modify their DNR orders at any time, as long as they are competent to make such decisions.
-
All healthcare providers must honor a DNR order.
In Texas, healthcare providers are generally required to respect a valid DNR order. However, there may be exceptions in certain emergency situations, and it's crucial to communicate your wishes clearly.
-
Having a DNR means giving up on life.
This is a common misunderstanding. A DNR reflects a person’s wishes regarding resuscitation, not their desire to stop all medical care or to hasten death.
-
A DNR can only be created in a hospital setting.
In Texas, DNR orders can be created in various settings, including at home or in long-term care facilities. It is important to ensure that the order is properly documented.
-
Family members can make DNR decisions without consent.
Family members typically cannot make DNR decisions on behalf of a patient unless they have been legally designated as a decision-maker. Clear communication and documentation of wishes are vital.
-
A DNR is the same as an advance directive.
While both documents relate to healthcare decisions, they serve different purposes. An advance directive covers a broader range of medical decisions, while a DNR specifically addresses resuscitation efforts.
-
Once a DNR is signed, it cannot be discussed again.
This is a misconception. It is important to revisit and discuss DNR orders regularly, especially as health conditions change or family dynamics evolve.
By clarifying these misconceptions, individuals can make informed decisions about their healthcare preferences and ensure that their wishes are respected.